Aggressive
form of prostate cancer ID’d by test
Finding may lead to better diagnostic tools for
disease
By MITZI BAKER
Prostate cancer is often a slow-grower that
doesn’t spread. In some cases, however, a deadly migration of
cancer cells invades other parts of the body. School of Medicine
researchers have now found a way to distinguish between the two
forms early, which may one day provide a test to determine when
invasive treatment is the best option.
Urology postdoctoral scholar Jacques Lapointe, MD, PhD, working
with senior study investigators Jonathan Pollack, MD, PhD,
assistant professor of pathology, and James Brooks, MD, assistant
professor of urology, scanned thousands of genes in normal and
diseased prostates and discovered that as few as two specific genes
appear to indicate which tumors will be aggressive and which will
not. Their findings were published in the Jan. 20 issue of the
Proceedings of the National Academy of Sciences.
“It is the first time we’ve been able to take tumors
that generally appear the same under the microscope and say that we
can see differences that appear useful in predicting how these
patients will fare,” said Pollack. This work is “early
translational research,” he emphasized, and will need to be
validated by other groups and through prospective clinical
trials.
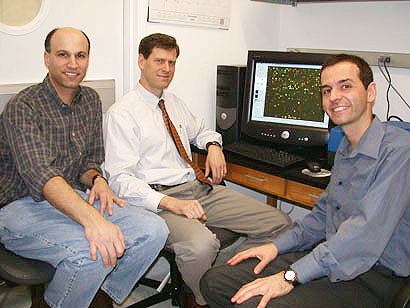
Jonathan Pollack, MD, PhD
(from left), James Brooks, MD, and Jacques Lapointe, MD, PhD, take
a break from studying microarray data identifying genes that
determine whether a case of prostate cancer will be slow-growing or
aggressive. Photo: Mitzi
Baker
Current techniques for estimating the severity of prostate cancer
include measuring the level of prostate specific antigen, or PSA,
and determining tumor stage and grade. These methods, said
Lapointe, provide limited information about both the progression of
the disease and the best course of action.
“We have the PSA blood test, which is not without
faults,” said Brooks, who provided prostate samples from his
patients who consented for the study. He explained that while the
PSA test has proved to be a useful tool in screening men for
prostate cancer, a number of less dangerous conditions can cause
the level of PSA to rise, which has opened controversy over the
test’s usefulness. An easily detectable indicator that not
only unequivocally tells if cancer is present but also how
aggressive it is would be ideal, he noted.
Using microarrays -- glass slides carrying more than 26,000 DNA
spots, each representing a different gene -- the group profiled
gene expression in 112 prostate samples to study the differences
between normal tissue and tumor tissue. They discovered that the
cancers fell into one of three subtypes based on which genes were
turned on or off. Two of these subtypes were associated with more
aggressive cancers.
Interested in streamlining the identification process, they tried
using only a couple of the genes that appeared to indicate either a
more or less aggressive type of tumor to use as markers. They chose
the genes MUC1 and AZGP1 and used a simple antibody test to screen
225 archived prostate samples that had accompanying information
about how each patient had fared on average eight years after their
prostates were removed.
Although there are hundreds of genes that differentiate the
subtypes on the molecular level, the group found that those two
genes captured a significant amount of this information. “We
have shown that these markers predict outcome very well,”
said Pollack. “These markers improve our predictions for the
recurrence of tumors months or years after surgery over and above
anything available now.”
Since as few as two markers are effective at predicting how serious
a tumor a man may have, the simple antibody test could someday be
used clinically to screen for those markers. “It’s much
easier to stain for two antibodies than it is to perform a DNA
microarray,” said Pollack. “This test has the potential
to provide clinicians with more information about how to treat
tumors in their patients.”
Lapointe added that as they continue to screen more samples, they
may find even more subtypes to further characterize and better
predict the course of prostate cancer.
This research was made possible through National Institutes of
Health and National Cancer Institute sponsorship, part of a larger
research grant of biochemistry professor and Howard Hughes Medical
Institute investigator Patrick Brown, MD, PhD. Brown developed
microarrays at Stanford and collaborated on the study.
Seven other Stanford investigators from the departments of
pathology, urology, health research and policy, statistics and
genetics contributed to this project. This study was part of an
international collaboration and included investigators from Johns
Hopkins University, Louisiana State University and the Karolinska
Institute in Sweden.

|
Researcher
challenges value of widely used prostate cancer diagnostic tool
(2/13/02)
Controversial
faculty finding gets nationwide airing (10/9/02)
|

