Wastewater could be the key to tracking more viruses than just COVID-19
Researchers have developed methods for using wastewater to track the levels of various respiratory viruses in a population. This can provide real-time information about virus circulation in a community.
Public health experts commonly track spikes in flu, respiratory syncytial virus (RSV), and rhinovirus circulating in a population through weekly reports from sentinel laboratories. These laboratories process samples from only severely ill patients, and it can take weeks for the results to get into the database. Now, for the first time, researchers at Stanford University, in collaboration with Emory University and Verily Life Sciences, have collected fast and accurate readings of a whole suite of respiratory viruses in their local Santa Clara sewer system.
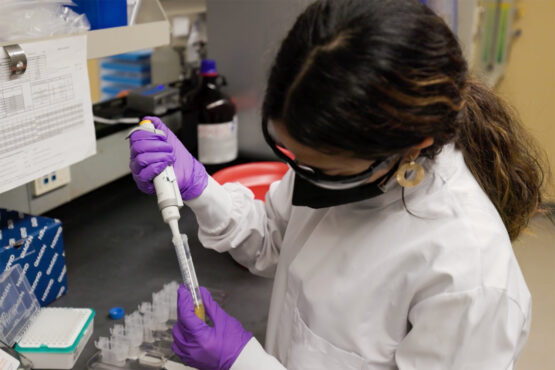
Boehm lab graduate student Winnie Zambrana showing how wastewater samples are processed to test for evidence of viruses. (Image credit: Harry Gregory)
Wastewater is currently the only source for accurate information about COVID-19 rates in communities. PCR testing is no longer widely available, and most people swab themselves at home where their results never reach public health agencies.
Prior to COVID-19, respiratory viruses had not been tracked through wastewater. Most of the viruses the scientists tested for in this study had never been measured in wastewater before. The findings are published in the March 22 issue of The Lancet Microbe.
“We are gathering evidence that wastewater can be useful for many infectious disease targets beyond COVID-19, and that it’s a really valuable resource for understanding community health,” says Alexandria Boehm, professor of civil and environmental engineering at Stanford Engineering and the Stanford Doerr School of Sustainability. “We found that concentrations of RNA, the building block of virus genomes, from influenza A and B, RSV, rhinovirus, parainfluenza, metapneumovirus, and seasonal coronaviruses in wastewater follow the trends also observed in the clinical data from sentinel laboratories. The possibilities seem very endless at this point.”
Boehm envisions a future where communities could continually test wastewater for all kinds of viruses. With up-to-the-minute virus reports, calculating our risk for flu that day would be as easy as checking the local weather forecast for rain.
Looking beyond COVID-19
Sputum, mucus, feces, and urine all enter the wastewater every time we use a drain in the house or at the office, carrying viruses and bacteria along. When researchers take a sample of wastewater, they get a giant biological sample from the entire toilet-flushing, toothpaste-spitting, shower-taking population. That sample contains contributions from all individuals, even those who may be mildly ill or even asymptomatic.
If the local treatment plant processes wastewater from a city of a million people, a single sample provides scientists with information about all those people. Researchers can see the infectious diseases circulating in the population and observe how the infections are changing over time in the community.
Given that wastewater is an ideal source to study COVID-19 cases, Boehm and her colleagues decided to see if they could also use wastewater to understand circulation of other respiratory viruses. “That motivated us to do this study and develop assays for all these different respiratory viruses and see if they tracked the data that was available for the state of California on circulation of these viruses in clinical samples,” Boehm says.
Boehm’s team discovered that the concentrations of the viruses they measured in local wastewater matched the state of California’s clinical data of the relative infection rates of the viruses. In other words, when the state data suggested that there were a lot of people suffering from seasonal coronavirus infections, those spikes showed up in wastewater too.
“This suggests that wastewater can be used to understand the circulation of these respiratory viruses at a more local scale than at the state level with the clinical information,” says Boehm. “In addition, results on virus circulation can be real time.”
Quick and easy to implement
Boehm’s group runs a regular wastewater virus surveillance program with a team from Emory University and Verily Life Sciences. Setting up tests for new viruses in the program is straightforward with the sampling and testing infrastructure already in place. Researchers simply take the same samples and apply different assays to them to get information about more respiratory viruses, such as influenza.
The data from wastewater can be available within 24 hours of collecting a sample – faster than public health officials can get their hands on any clinical data. At this speed, public health departments can promote timely vaccinations, design education campaigns, and send warnings to vulnerable people about precautions they could take to avoid catching a specific disease.
Real-time data could also help medical doctors make decisions about testing and treatments. If a doctor knows that there’s no flu going around, they don’t need to waste a patient’s time and money on a flu test. Hospital directors could use more accurate virus information to help stock therapeutics in the hospital if they’re anticipating an outbreak.
“We envision something similar to a weather report where everybody could make their own decisions based on their own levels of risk that they’re willing to take and also their own health,” says Boehm. “Somebody who is undergoing chemotherapy could make their own decisions about masking or going to the grocery store, based on their understanding of what illnesses are circulating in the community.”
Boehm hopes this study will motivate more researchers to look for these infectious disease targets in wastewater across the country. “I think it’s really important to show that this works in more than one location, which I totally expect it will,” says Boehm.
Once Boehm and her colleagues have confidence that a virus they measure can be useful and meaningful, they can incorporate it into their larger WastewaterSCAN project data.wastewaterscan.org. “One of the most exciting things about wastewater monitoring is how quickly we can bring our innovations into practice,” says Marlene Wolfe, BA ’11, co-author on the study and assistant professor of environmental health at Emory University, “because we are already working with utilities and public health departments around the country, we can introduce new tests very quickly once we have the evidence that the wastewater data reflects community levels of disease.”
The research team is already studying the feasibility of monitoring more infectious disease targets in wastewater, including other respiratory and gastrointestinal viruses such as norovirus, adenoviruses, and enteroviruses. They are also working closely with public health officials to pinpoint more viruses, fungi, and bacteria to study, Boehm says. “We just need to keep doing research and exploring how far we can take wastewater surveillance for infectious disease targets.”
Boehm is also a professor of Oceans Department of the Stanford Doerr School of Sustainability, a senior fellow in the Stanford Woods Institute for the Environment, a member of Bio-X, a member of Maternal & Child Health Research Institute, and a faculty fellow in the Center for Innovation in Global Health.
Study co-authors include Marlene Wolfe, a former postdoc at Stanford University in the Department of Civil and Environmental Engineering and the Stanford Woods Institute for the Environment, and now an assistant professor of environmental health in the Gangarosa Department of Environmental Health, Rollins School of Public Health, Emory University; and researchers at Verily Life Sciences.
The study was funded by the CDC Foundation.
