Stanford researchers develop tiny nanostraws to deliver molecules to human cells safely and efficiently
Minuscule nanostraws could help solve the problem of how to deliver precise doses of molecules directly into many cells at once.
Researchers can design the perfect molecule to edit a gene, treat cancer or guide the development of a stem cell, but none of that will matter in the end if they can’t get their molecule into the human cells they want to manipulate. The solution to that problem, described in a study published October 31 in Science Advances, could be minuscule nanostraws, tiny glass-like protrusions that poke equally tiny holes in cell membranes to deliver their cargo.
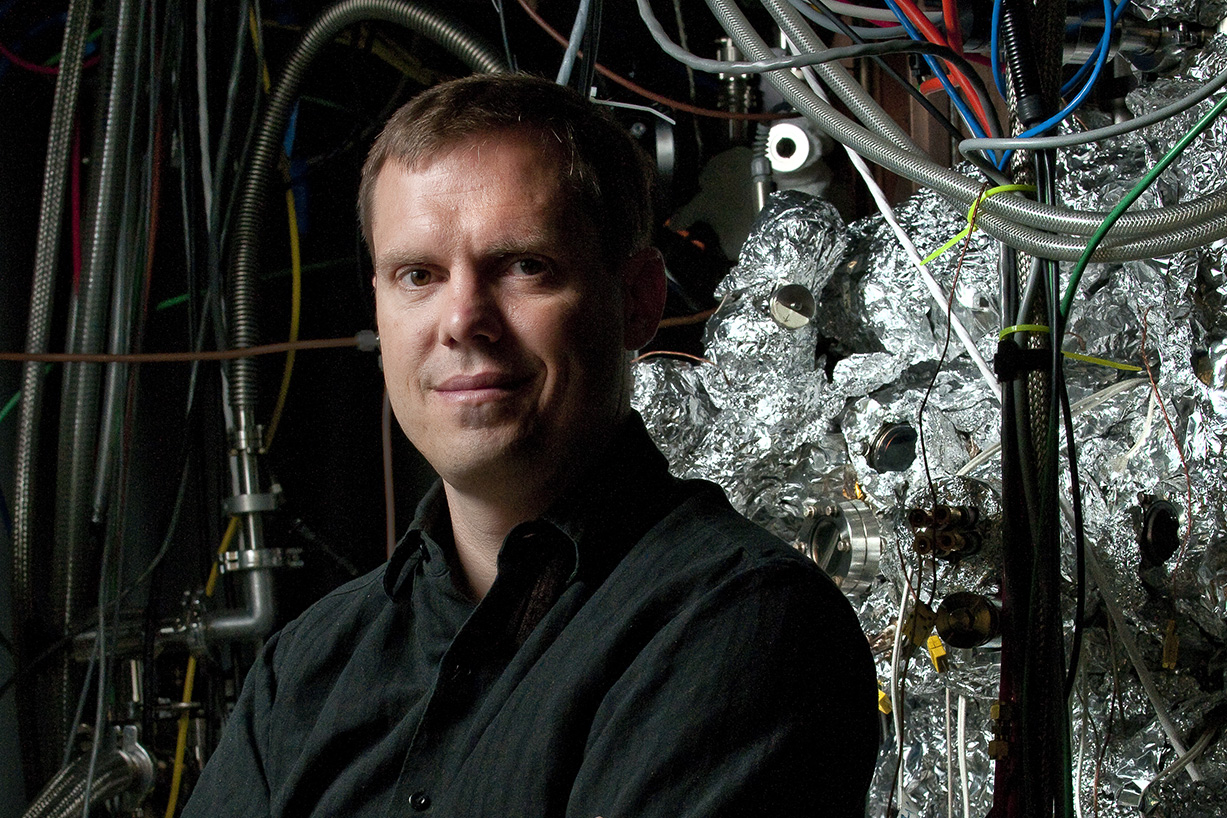
A team led by materials science engineer Nicholas Melosh has developed tiny nanostraws that can deliver molecules into cells more precisely, faster and safer than other methods. (Image credit: L.A. Cicero)
A team led by Nicholas Melosh, an associate professor of materials science and engineering, first began testing nanostraws about five years ago using relatively tough cell lines derived from cancers, mouse cells and other sources. Now, Melosh and colleagues have shown the technique works in human cells as well, a result that could speed up medical and biological research and could one day improve gene therapy for diseases of the eyes, immune system or cancers.
“What you’re seeing is a huge push for gene therapy and cancer immunotherapy,” said Melosh, who is also a member of Stanford Bio-X, Stanford ChEM-H and the Wu Tsai Neurosciences Institute, but existing techniques are not up the challenge of delivering materials to all the relevant human cell types, especially immune cells. “They’re really tough compared to almost all other cells that we’ve handled,” he said.
Crossing the cell membrane
The idea of transporting chemicals across the cell membrane and into the cell itself is not new, but there are a number of problems with the methods scientists have until now relied on. In one common method, called electroporation, researchers use an electric current to open up holes in cell membranes through which molecules such as DNA or proteins can diffuse through, but the method is imprecise and can kill many of the cells researchers are trying to work with.
In another method, researchers use viruses to carry the molecule of interest across a cell membranes, but the virus itself carries risks. While there are similar methods that replace viruses with more benign chemicals, they are less precise and effective.
That was the state of affairs until just five or six years ago, when Melosh and colleagues came up with a new way of getting molecules into cells, based on Melosh’s expertise in nanomaterials. They would use electroporation, but do it in a vastly more precise way with nanostraws, which because of their relatively long, narrow profile help concentrate electric currents into a very small space.
At the time, they tested that technique on animal cells sitting atop a bed of nanostraws. When they turned on an electric current, the nanostraws opened tiny, regularly sized pores in the cell membrane – enough that molecules can get in, but not enough to do serious damage.
The electric current served another purpose as well. Rather than waiting for molecules to randomly float through the newly opened pores, the current drew molecules straight into the cell, increasing the speed and precision of the process. The question at that time was whether the technique would be as effective on the kinds of human cells clinicians would need to manipulate to treat diseases.
Faster, safer, more precise
In the new paper, Melosh and team showed that the answer was yes – they successfully delivered molecules into three human cell types as well as mouse brain cells, all of which had proved difficult to work with in the past.
What’s more, the method was more precise, faster and safer than other methods. The nanostraw technique took just 20 seconds to deliver molecules to cells, compared with days for some methods, and killed fewer than 10 percent of cells, a vast improvement over standard electroporation.
Melosh and his lab are now working to test the nanostraw method in some of the hardest to work with cells around, human immune cells. If they succeed, it could be a big step not just for scientists who want to modify cells for research purposes but also for medical doctors looking to treat cancer with immunotherapy, which right now involves modifying a person’s immune cells using viral methods. Nanostraws would not only avoid that hazard but could potentially speed up the immunotherapy process and reduce its cost as well, Melosh said.
Melosh is also an associate professor of photon science. Additional Stanford authors include Richard Lewis, a professor of molecular and cellular physiology; Joseph Wu, the Simon H. Stertzer, MD, Professor and a professor of radiology; postdoctoral fellow Ruoyi Qiu; and graduate students Yuhong Cao and Angela Zhang.
The research was funded by grants from the National Institutes of Health, the National Science Foundation, the Knut and Alice Wallenberg Foundation and the Wu Tsai Neurosciences Institute.
