Stanford Biodesign marks 15 years with new name, focus
Program has been renamed the Byers Center for Biodesign, and it’s now focusing on creating health-care technology that’s affordable.
As a specialist in heart rhythm problems, Uday Kumar always thought there had to be a better way to monitor the cardiac rhythm activity of his patients when they were outside the clinic, going about their usual activities. Traditionally, patients were prescribed a camera-size device, hooked to their bodies via electrodes, to track their heart rate during the day and while sleeping.
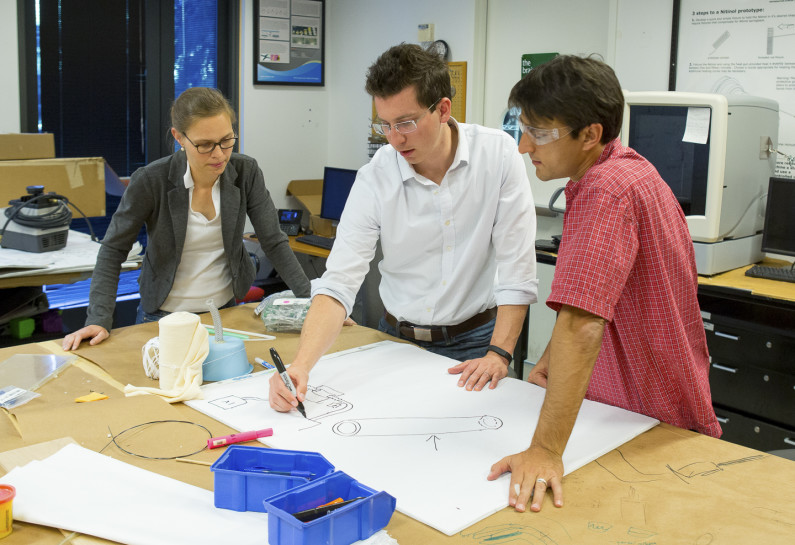
Bioengineering postdoc Veronique Peiffer and graduate student Richard Timm work with lecturer Ross Venook on ideas for solutions to unmet health-care needs. (Image credit: Norbert von der Groeben)
These devices have been around for decades, “but they are cumbersome and difficult to use,” said Kumar, a consulting associate professor of bioengineering. “I think this is a need that people had overlooked for a while: something you could use to monitor patients with a suspected arrhythmia that is more cost-effective and easier for the patient to use.”
As a fellow in the Stanford Biodesign Program in 2005-06, Kumar set his sights on finding a more cost-effective, user-friendly solution. His invention, the ZioPatch, which has been worn by more than 400,000 patients, is one of dozens of devices to emerge from the program’s innovation process, which has become the international model for inventing new medical technologies.
Focus on affordability
This year, the program celebrates its 15th anniversary. It has been renamed the Stanford Byers Center for Biodesign and is moving forward with an emphasis on creating new health technologies that not only benefit patients, but also take into consideration the economic challenges of health care today, said Paul Yock, founder and director of the program at Stanford.
“We have been very successful in training high-tech innovators in the last 15 years,” said Yock, a professor of bioengineering and of medicine, who is a successful inventor himself. “Going forward, with the monumental changes in health care and the many cost pressures on the system, we need to create technology that enhances care and does it in a way that’s not unduly expensive. That is a sea change.”
The center is being renamed in honor of longtime Silicon Valley venture capitalist Brook Byers, who has mentored, coached and supported fellows since the program’s inception.
“This program is uniquely positioned to improve human health around the world,” Byers said. “Their fellows and medical innovations change health care and have already directly benefited hundreds of thousands of patients. And they’re inspiring and empowering others by sharing best practices globally.”
Legacy of inventions
Since the program’s launch in 2001, it has trained more than 1,000 graduate students and nearly 200 fellows. The trainees have founded more than 40 companies and created products used by well over a half-million patients, said Yock, who is also the Martha Meier Weiland Professor in the School of Medicine. These include devices to forestall night terrors in children, prevent infections after surgery, relieve symptoms from an enlarged prostate, provide respiratory support in low-resource settings, as well as to treat dry eyes and women’s incontinence.
“Biodesign is a program that exemplifies the concept of precision health. Working at the intersection of medicine, engineering and business, Biodesign fellows are delivering path-breaking solutions to the most pressing human health problems,” said Lloyd Minor, dean of the School of Medicine. “Moreover, these innovative fellows go back out into the world, taking with them not just their first invention but their capacity to keep inventing – and to teach others how to invent – whether in their own startups, in existing companies or as faculty members in top universities. This is the multiplier effect: We seed the world with people who approach innovation using this proven, needs-based process.”

Uday Kumar, director of strategy, and Lyn Denend, director of academic programs, discuss the mission of the new Stanford Byers Center for Biodesign.
“Over the last 15 years, Stanford Biodesign has had an extraordinary impact on the world,” said Persis Drell, dean of the Stanford School of Engineering. “It has done so in large part because its leadership recognized early on that solving big, complex problems requires teams of scholars from multiple backgrounds and disciplines to work together. Stanford engineers are very proud to be a part of this highly successful collaboration and look forward to continuing to do so.”
The program had its genesis in the late 1990s when Stanford Bio-X, the university’s interdisciplinary biosciences institute, was taking shape. Yock was among a dozen faculty in medicine and engineering with an interest in medical technology innovation who wanted to create a unit within Bio-X, he said. The group was committed to having a fellowship training component in the program and reached out to Josh Makower, a successful medical technology entrepreneur who had developed an interdisciplinary training initiative while at Pfizer. With help from faculty and industry colleagues, Makower developed the Stanford training approach and became the program co-founder and its first fellowship director.
The new program moved from its temporary headquarters in the Center for Clinical Sciences Research into the James H. Clark Center, the Bio-X hub. Initial funding was provided by a combination of private donors and industry gifts, followed by foundation and grant support, and the program continues to rely on these funding sources today.
In 2003, Tom Krummel, then chair of surgery and a robotics expert, became co-director of the program and actively began recruiting surgeons as fellows. Currently, surgeons will often spend two years, rather than one year, at Biodesign because the second year is when most surgical inventions take on a life beyond the theoretical, Krummel said. “By the second year, the fellows are much closer to having not just a technology but the ability to build a sustainable business,” he said.
Identifying unmet needs
The program selects 12 fellows each year from an international pool of candidates and divides them into teams of four – typically two physicians and two engineers.
For all the fellows, the training process begins with the critically important step of identifying an unmet clinical need, said Makower, a consulting professor of medicine at Stanford. He believes many companies fail at innovation because they start first with a technology and then try to find a place where it might be put to clinical use. But technology will only make meaningful, lasting improvements in how health care is delivered if it addresses a clear need, he said.
To identify compelling needs, the fellows spend two months observing patient care at Stanford’s hospitals and clinics, soaking up the clinical experience. As the first fellowship director, Makower said he encouraged fellows to sleep in the residents’ on-call room so they could observe every step of the clinical interaction and even visit patients’ homes when possible and appropriate to see how they were adhering – or not adhering – to a particular therapy.
During this time, the fellows may identify as many as 200 needs. Then they have to select the two or three that seem most promising, and ultimately choose just one of them.
In the past, Yock said, cost wasn’t a primary consideration, but that has changed as a result of increasing pressure from government and private payers.
“We never paid much attention to how much our inventions would cost – or cost the system,” he said. “Now we teach the fellows that it’s essential to take economics into consideration before, during and after they invent. That’s true for the United States’ health-care system and in the global health-care environment, where affordability is an even more important factor.”
Taking a hard look
At this stage, too, the fellows have to take into account many other issues that could influence whether a device is successful.
“You have to ask, ‘Is there a clear regulatory path?’” said Kumar, now the program’s director of strategy. “What is your pathway to reimbursement and is it feasible? Can you protect the intellectual property? What business model will provide sustainability? Is there global play beyond the U.S.?
“Most needs and solutions don’t hit all of those,” he said. “The challenge is not to fall in love with any one idea but objectively take a hard look and find the one that has the best chance of reaching patients once you take all of these factors into account.”
Once fellows have settled on an idea, they begin the process of implementing their solution, possibly developing a prototype and building a plan to help bring it to the marketplace.
To help the fellows better understand the universe of medical technology, the program brings in experts from various fields, including regulatory and patent experts, venture capitalists and marketing specialists, who donate their teaching time, Makower said.
Drawing on these outside advisers “has really crystallized the whole community around the program,” he said.
Stanford faculty also teach in the program, which offers one- and two-semester classes for graduate students in medicine and engineering, as well as a courses for undergraduates.
Interest from abroad
Over the years, the program has attracted considerable interest from abroad, leading to collaborations in India, Ireland and Singapore. More recently, Stanford Biodesign helped initiate a program in Japan, which was announced last year by Prime Minister Shinzo Abe on his visit to the Stanford campus. Innovators trained in these international programs are developing life-changing solutions tailored to the specific needs of patients in their communities.
Through these partnerships, particularly in India and Southeast Asia, “we are trying to absorb their culture of cost-effective innovation,” Yock said, and benefit from the experience of entrepreneurs who may live and work in a resource-limited environment. He and his colleagues maintain ongoing relationships with program alumni abroad as they invent and develop technologies and build biodesign training programs in their home countries.
“We are moving the entire fellowship to a more global orientation and will be accepting fellows from any country on a ‘best athlete’ basis,” Yock said. The program will expose future fellows to global markets during their training through lectures and visiting speakers, and help make connections for those who want to go to the developing world after their fellowship year.
Yock and his colleagues also have documented the discipline of the biodesign innovation process in a textbook, a 2-inch thick resource that he edited with Makower; Stefanos Zenios, a professor at the Stanford Graduate School of Business; and a team of others. The textbook is being used as a teaching tool in scores of major universities around the world, helping cement the center’s role as a global leader. Yock also helped launch the Biomedical Innovation Engineering, Design and Entrepreneurship Alliance, a group of faculty at 100-plus universities who share experiences, challenges and opportunities to advance training in biomedical engineering and innovation.
Makower said the business of developing new medical technology is a tough one, as there may be hundreds of failures for every success. And the profits are modest compared to an Internet or social networking megahit, he said. But the payoff in human terms is enormous.
“When you invent a device that addresses a compelling medical need and someone is successfully treated,” he said, “there’s nothing better than that.”
